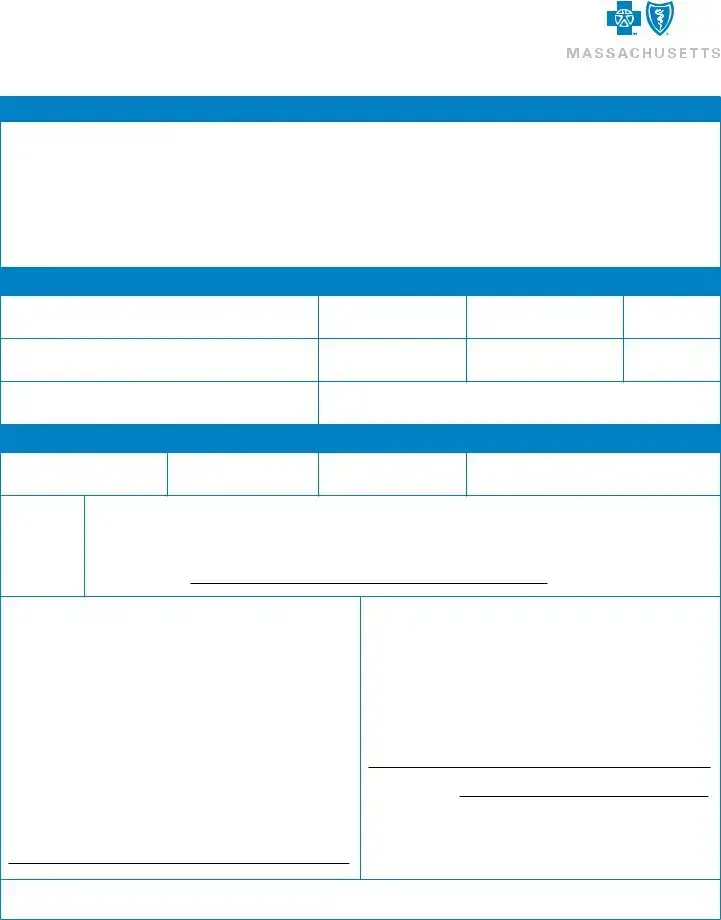
What is the correct way to submit a claim to Blue Cross Blue Shield of Massachusetts (BCBSMA)?
To properly submit a claim to BCBSMA, follow these steps: Begin by ensuring you are submitting the claim for a service from a provider who does not directly submit claims to BCBSMA. Complete a separate claim form for each patient involved. Attach the original, detailed bill from your healthcare provider to the form. It’s essential to retain copies of all submitted documents for your records because original documents will not be returned. Ensure that your claim form is signed and dated, and then mail it along with all required attachments to the designated address: BCBSMA, P.O. Box 986030, Boston, MA 02298.
What should I do if the patient has other insurance plans in addition to BCBSMA?
If the patient is covered by other insurance plans besides BCBSMA, indicate this on the claim form by marking "Yes" where it asks if the patient has other insurance and provide the necessary details. This includes Medicare parts A, B, or D, other Blue Cross Blue Shield memberships, or any other insurance plans. Include the identification number and name and address of the other insurer. This information helps in coordinating benefits and ensuring that all sources of coverage are considered.
How do I know if my claim form has been processed?
To check the status of your submitted claim, you can visit the BCBSMA website. If you haven't already, you will need to create an account on Member Central. Once registered and logged in, you will have access to view processed claims and gain insights into the status of your submissions. Typically, allow up to 30 days for the claim processing to complete.
What information is required on the itemized bill from my provider?
An itemized bill from your provider must include several critical pieces of information to be considered complete. It should be on the provider's letterhead, encompassing the provider's name, address, Tax ID/NPI, and credentials. The patient’s name, dates of service, detailed charges for each service, procedure codes, diagnosis codes, and the number of units for services rendered are also required. For treatments like occupational, physical, and speech therapies, as well as anesthesia and chiropractic services, specifying the number of units is particularly crucial. When submitting a claim for prescription drugs, an itemized receipt from your pharmacy that includes the National Drug Code, drug name, date dispensed, quantity, and prescribing physician's name must be provided.
What steps should I take if my claim involves services due to an accident?
If the services you are claiming are the result of an accident, whether it’s an auto accident, work-related accident, or other types of accidents, you should indicate this on the form by marking "Yes" in the appropriate section and provide the date of the accident. For auto accidents, also include the name of your auto insurance and your policy number. This information is crucial for determining whether other insurance or parties are responsible for covering some or all of the costs of the care provided.
Is it necessary to include Medicare information on the claim form?
Can I submit a claim form for a dependent?
Yes, you can submit a claim form for services rendered to a dependent. When completing the form, specify the relationship of the patient to the subscriber by selecting the appropriate option, such as spouse, child, student age 19 or older, or handicapped dependent age 19 or older. It's important to complete a separate form for each patient, even if they are dependents covered under the same health plan.
What should I do if I have questions about completing the claim form or if I encounter issues during the process?
If you have any questions or face difficulties while completing the claim form or during any part of the claim submission process, you should contact BCBSMA customer service for assistance. They can provide detailed guidance and support to help ensure your claim is completed properly and processed efficiently. Contact information is available on the BCBSMA website, and customer service representatives are equipped to assist with any inquiries you may have.